Halitosis, or bad breath, is a common condition in oral health care that affects people of all ages and can decrease self-confidence and social interactions. Estimations state that 50% of people experience halitosis regularly.
“Most of my patients are timid when talking about bad breath. My approach is discussing the mouth and body as a whole versus separate entities and helping the patient maximize their overall health. This is because bad breath is usually associated with sub-optimal health in some form. It's important for me to understand the underlying issue to devise treatment solutions for their bad breath." – Dr. Chris Strandburg, DDS
Since bad breath can be not only annoying but also hazardous to our health, it is vital to introduce new oral hygiene recommendations and proper oral health care rituals.
Let's take a closer look at what causes bad breath and what we can do to keep our breath fresh.
Most common causes of halitosis
The sources of halitosis fit two categories: intraoral (in the mouth) and extraoral (from outside the mouth).
Below we will explore the most common causes of intraoral and extraoral halitosis.
Intraoral halitosis
Intraoral halitosis is responsible for approximately 90% of halitosis cases. It’s caused mainly by a buildup of molecules called volatile sulfur compounds (VSCs), which have an unpleasant odor.
VSCs include hydrogen sulfide (which has a rotten egg smell) and methyl mercaptan (producing a bad cabbage smell). When VSCs build up in our mouths, their unpleasant odor diffuses as we breathe and speak.
Factors that influence the levels of VSCs in our mouth include oral bacteria, oral disease, tongue coating, and dry mouth.
Oral bacteria
Our mouths are filled with bacteria, fungi, and viruses – collectively called our oral microbiome. Most of these species are beneficial and help us extract vitamins from our food, fight off infection, and even reduce our blood pressure and increase our cognitive function. But some species are harmful and lead to conditions like bad breath, cavities, and gum disease if they grow too large in number. More and more dentists recommend frequent oral bacteria tests to prevent bacteria-related diseases.
Oral bacteria are the primary producers of VSCs in our mouths. Certain species, including S. moorei, P. gingivalis, and P. nigrescens, break down proteins in our diet and release VSCs as a byproduct – leading to bad breath. Studies have found direct associations between the levels of these species and the amount of VSCs they produce.
As these bacteria build up they arrange themselves into a community structure called a biofilm. This all starts with individual bacteria colonizing our teeth, which can take place minutes after a professional cleaning. Hours later, this turns into biofilm, and during the rapid growth stage, the bacteria (biofilm) starts to multiply throughout the mouth.
You can typically feel this biofilm as a slimy coating on your teeth or tongue. These bacteria are anaerobic, which means they cannot survive in oxygen. Forming this biofilm allows them to create a protective layer from oxygen and disturbances to continue multiplying. As this biofilm develops further, it will harden into dental plaque on our teeth and gums, a coating on our tongues, or “stones” on our tonsils, making it harder to remove.

Gum disease and plaque
The bacteria that cause gum disease (gingivitis and periodontitis) are also associated with the production of VSCs. When we don’t practice proper oral hygiene, these bacteria build up beneath our gumlines and around our teeth and release toxic byproducts.
Some of these byproducts trigger inflammation, which, over time, will lead to gingivitis and, if left untreated, periodontitis. As our gums become inflamed, a space between our gums and the tooth will form, known as “pockets”. The larger the pocket is, the more bacteria can develop and create havoc in the oral cavity, leading to further inflammation and VSC production.
Tongue coating
The most common home for halitosis-causing species is the tongue, particularly towards the back (closest to the throat). As bacteria build up, they assemble into a biofilm on the tongue and form a coating.
Tongue coating microbiota can offer essential clues in investigating the pathogenesis and treatment of halitosis. The tongue has small hair-like projections called filiform papillae on top of it, creating an ideal habitat for bacteria. Much like ants in a deep-pile rug, bacteria can hide between these hair-like projections and thrive. Eventually, the bacteria colonies multiply into a “film” or coating on the tongue. The bacteria within this film create many of the odor-causing VSCs that lead to halitosis.
Tonsilloliths (Tonsil stones)
Another place halitosis-producing species colonize is our tonsils. They will arrange themselves into a biofilm that can eventually harden (calcify) into tonsilloliths, also called “tonsil stones”, attached to our tonsils and can cause a lingering unpleasant odor in the mouth. Studies examining tonsilloliths have found they have a similar structure to dental biofilms (like plaque). A dental or medical professional examination diagnoses tonsilloliths.
Dry mouth
A common reason for bacterial buildup and subsequent bad breath is having decreased saliva (hyposalivation). Individuals with low salivary production have significantly higher levels of VSCs. In addition, the presence of tongue coating and stones rises compared to individuals with a regular salivary flow.
One reason for this is harmful bacteria can typically only survive in our mouth if they manage to hold on and not get swallowed. Saliva contains proteins that stick to the bacteria and act as a natural rinse to remove them. These proteins include lysozymes that attack bacteria's cell walls and make them burst, and antibodies, that prevent bacteria from settling onto our teeth and tongue.
Saliva also helps promote beneficial bacteria that help control the levels of harmful species known to cause cavities, gum disease, and more. Saliva extracts nitrate from our diets and feeds healthy bacteria, called nitrate-reducing species, helping to produce nitrous oxide, which aids in lowering blood pressure and increasing cognitive function. In addition, these species naturally release low levels of hydrogen peroxide and other byproducts, which kill the bacterial species associated with halitosis and gum disease.
When we sleep, our saliva flow nearly stops, which is one reason why bad breath is most common when we first wake up. Other causes of dry mouth include certain medicines, drinking alcohol, dehydration, and missing meals – the act of chewing increases saliva in the mouth.
Extraoral halitosis
Up to 15% of all bad breath cases are extraoral – resulting from infections outside the mouth. For example, ear, nose, throat, or respiratory diseases (like sinusitis or tonsillitis) or foreign bodies (like stuck food) in the airway can cause bad breath.
Specific chronic diseases like gastric reflux, diabetes, carcinoma, and liver or kidney disease and medications may also result in extraoral halitosis.
Diet and lifestyle
Certain diets can lead to temporary halitosis. Garlic and onions contain high levels of sulfur compounds that can linger in our mouths and enter our bloodstream, leading to odor when we exhale. Coffee and alcoholic beverages can also temporarily change the scent of our breath and can lead to or worsen dry mouth symptoms.
Low-carb, high-fat diets, like Keto diets, can also lead to halitosis. The goal of these diets is to restrict carbohydrate intake to force it to burn fat for energy, releasing ketones as a natural byproduct. Ketones include beta-hydroxybutyrate, acetoacetate, and acetone – which also cause bad breath.
H. Pylori infection
Another proposed source of extraoral halitosis was the presence of H. pylori in the gut or oral microbiome. H. pylori is an infection in the digestive system which breaks down the stomach lining and acidity levels, which help us fight diseases.
Around 44% of people worldwide have an H. pylori infection. Harmful bacteria buildup can increase, and with symptoms of vomiting, burpìng, and poor diet, saliva levels drop, and halitosis can occur.
GERD
Gastroesophageal reflux disease (also known as GERD or acid reflux) occurs when stomach acid frequently flows up into the tube connecting your mouth and stomach (esophagus). This backwash can irritate the lining of your esophagus.
Symptoms of GERD include bad breath. Possible explanations for this relationship are that the odor may result from the accumulation of postnasal drip on the back of the tongue. In GERD, acidic stomach contents can reach the top of the throat and irritate the throat walls, resulting in postnasal drip. Another explanation is that intestinal gas and stomach contents may release through the esophagus due to a damaged lower esophagus, typically responsible for limiting these contents from coming up from the stomach.
How to treat bad breath?
Oral hygiene
The first best defense against bad breath is understanding the importance of oral health care and practicing proper oral hygiene, such as regular brushing and flossing or other interdental (between the teeth) cleaning methods, like using an oral irrigator. Following consistent oral hygiene recommendations, we can prevent oral bacteria from forming odor-causing biofilms on our teeth, gums, and tongue.
A systematic review of clinical trials found that professional teeth cleaning, scaling, and root planing (deep cleaning), combined with oral hygiene practice, reduced the levels of VSCs in patients with intra-oral halitosis or gum disease. Independent of tongue cleaning or mouth rinse use. However, routine oral hygiene may not be sufficient to prevent or cure halitosis.
Tongue cleaning or tongue scraping
Regular tongue cleaning can reduce the levels of VSCs in people with halitosis from 30-75%.
In 2001, scientists assessed the effectiveness of different tongue cleaning devices in reducing oral VSC levels. They used a combination brush and scraper, a tongue scraper, and a regular toothbrush. The oral bacteria tests presented a 42%, 40%, and 30% reduction in VSCs, respectively.
The decrease in VSC lasted significantly longer in subjects who used the tongue cleaner; yet, after more than 30 minutes, the reduction in all cases was undetectable. Oral hygiene recommendations include, but are not limited to, the removal of bad bacteria. The importance of oral health care in increasing good bacteria is vital.
Mouthwash
There are several types of mouthwash that have received the ADA seal of acceptance and are clinically-approved oral hygiene recommendations. These mouthwashes contain different active ingredients to reduce the bacterial abundance and the VSCs that they produce.
Systematic reviews found mouthwashes that contain chlorhexidine (CHX), cetylpyridinium chloride, and zinc reduce halitosis. At three and six months, individuals using the zinc acetate/CHX rinse showed significant reductions in the total VSCs in their oral bacteria test. With regular rinsing, the study group showed no differences in tooth staining.
However, long-term use of CHX mouthwash has potential disadvantages, including teeth and tongue staining, a metallic sensation, or reduced taste.
The above mouthwashes simply reduce the abundance of bacteria and kill diversity. Without an oral bacteria test, it’s challenging to know what bacteria is present and what quantity of harmful or good species the mouthwash removes. Halitosis sufferers can consider mouthwashes as a short-term solution and combine it with other oral hygiene recommendations. Their microbiomes need to be re-seeded with strains that support oral health.
Oral Probiotics
Several studies have looked into the efficacy of probiotics in reducing symptoms of halitosis and VSC producing species of bacteria, with promising results.
One study sought to measure oral bacteria tests, and the effects of probiotic species S. salivarius strains K12 and M18 in culture. They isolated two species associated with VSC production and gum disease, P. gingivalis and T. denticola, and cultured them with and without K12 and M18. The study found the culture with high concentrations of K12 and M18 significantly reduced the VSC levels produced and reduced P. gingivalis and T. denticola by roughly 50%.
Other studies have measured the effects of oral probiotics in controlled patients, with and without other interventions like mouthwash and tongue scraping. It looked into the effects of probiotics in individuals with tongue coating.
Probiotics case study: combined treatments
Scientists split twenty-eight subjects with tongue coating into two groups, with fourteen using a probiotic tablet for 30 days while the others took a placebo. Both groups continued their standard oral hygiene regimens but did not practice tongue scraping. The scientists took the patient’s oral bacteria tests one, seven, and fourteen days after and inspected the results.
On day one, the probiotic group had significantly lower levels of VSCs and reduced tongue coating than the placebo group. However, they had no statistically significant differences in VSC levels and tongue coating on days seven and fourteen. The study concluded that patients might require physical or chemical removal of the tongue coating before probiotic use.
Supported by a separate study that looked into the effectiveness of probiotic use in combination with tongue scraping, this study split 100 participants into three groups: one that performed tongue scraping (TS); a second that performed TS and used a probiotic (PB); and a third that did not TS but rinsed their mouths for two minutes with water after brushing (MW). They took measurements after one month of treatment, then one month after stopping treatment.
The TS-only group significantly decreased halitosis in the first month, but levels rose again in the final measure. The PB group showed significant drops in halitosis measures in the first month and sustained their low levels after stopping treatment. The MW group presented no difference throughout the study.
These findings suggest that adding a probiotic to a thorough oral hygiene routine helps improve oral health in a more lasting way than one oral hygiene recommendation alone. Thus, it is not enough to simply remove harmful bacteria with mouthwash – we must promote beneficial bacteria to take their place.
Increase saliva production
Individuals struggling with dry mouth can consider several options to increase their saliva production. Oral hygiene recommendations include chewing a sugar-free or xylitol gum and xylitol lozenges.
Similarly, xylitol-containing mouthwashes like Biotene Dry Mouth Oral Rinse or ACT Total Care Dry Mouth mouthwash support saliva production and prevent bad breath. Xylitol is a natural sugar alcohol found in plants, including many fruits and vegetables, that can reduce harmful bacteria in our mouths.
The intake of alcohol, caffeine, and mouthwashes that contain alcohol also leads to dry mouth. Limiting these substances can also improve oral health care and overall health.
Diet
Proper hydration with water can further help to stimulate saliva production and remove food particles from our mouth that feed VSC-producing bacteria.
Raw fruits and vegetables high in fiber also reduce disease-causing bacteria, while yogurt can effectively promote probiotic bacteria and lower levels of VSCs.
For oral hygiene, the most highly recommended foods are nitrate-rich vegetables like spinach, lettuce, fennel, radishes, and beets. These act as a probiotic and increase the levels of beneficial bacteria in our oral microbiome.
Conclusion
In summary, oral bacteria in the gums, tongue, tonsils, and dry mouth – all known as intraoral halitosis causes – are the main sources of bad breath. However, diet, H. pylori, or a medical condition like GERD – extraoral halitosis – can also lead to bad breath. Treatments include tongue scraping, mouthwashes, increasing saliva production, and maintaining a healthy diet.
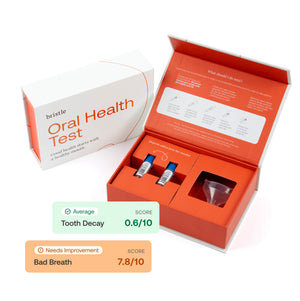
Want to learn more about your oral health, and if you have the bacteria that cause bad breath? You can test your oral bacteria with the Bristle Oral Health test.