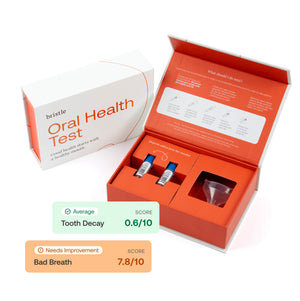
Bristle research digests are short research articles that share some of the insights around the oral microbiome and how it impacts health and disease. All data come from Bristle’s internal research, which leverages the Bristle Comprehensive Oral Microbiome Test, a saliva-based at-home test that measures microbes in the oral microbiome using shotgun metagenomic sequencing.
Background about gum disease
An estimated 47.2% of all American adults over 30 years old have periodontal disease, characterized by irreversible bone loss caused by inflammation of the gums. Decades of research has shown the causal relationship between the oral microbiome (the bacteria, fungi, and viruses in the mouth), and periodontal disease. For decades, specific pathogenic bacteria have been isolated from gums and plaque of patients with disease.
We looked at whether these pathogens were present in saliva from people with gum disease versus healthy people. Using machine learning, we developed a model to predict incidence of gum disease using only data from the salivary microbiome, and here provide evidence that the oral microbiome is a powerful tool to predict and monitor severity and potentially the progression of gum disease. This data may help enable future personalization of antimicrobial therapy for patients with gum disease before onset of irreversible bone loss.
The oral bacteria can be a predictor of gum disease
Each dot represents a single saliva sample from a different Bristle user. The boxplots show the 25th, 50th, and 75th quantiles for each group. The y axis from each plot shows a different score or abundance measurement, and the x-axis shows status of periodontal disease. The dots are jittered for easier visualization.
First we looked at the abundance of a dozen bacterial species across healthy and diseased individuals. These dozen species are commonly referred to as periodontal pathogens based on foundational research from Socransky (1). The first plot shows the relative abundance on the y-axis and periodontal disease status on the x.

In a second plot, we ranked bacterial species on a percentile scale (0 to 100) to normalize their relative abundances for easier comparisons.

As a control, we looked at 7 species not usually related to periodontal disease, 1 species associated with dental caries, and 1 microbe at the genus level. We found that many of the commensal species were reduced in people with periodontal disease, though not statistically significant. As expected, S. mutans was not different between groups.

The low prevalence of periodontal associated species was expected given that research shows that periodontal disease is polymicrobial rather than caused by a single species. Therefore, we hypothesized that the total number of detected species would be higher in people with gum disease compared to those without.

We found that of these 12 periodontal disease associated species, healthy people had an average of fewer than 4 detected species while people with gum disease had an average greater than 6. Using just those 12 species, we built a simple model to create a single score to describe risk of disease. As shown below, people with periodontal disease had significantly higher scores than healthy people.

Not surprisingly, we also found dozens of unique bacterial strains significantly increased in people with gum disease compared to people without (data not shown). To improve the model above, we applied machine learning to predict gum disease solely using biologically plausible bacterial strains from salivary oral microbiome data. The receiver operating characteristic curve for the model is shown below, exhibiting a AUC of 88.32.

Discussion
Our results demonstrate the utility of the salivary oral microbiome in identifying and quantifying pathogens related to gum disease. Decades of research have shown that periodontal associated pathogens drive inflammation and disease, and we show that the relative abundance of these pathogens in saliva is significantly higher in patients with disease than those with healthy gums.
The prevalence of these periodontal pathogens varies greatly from patient to patient. Many studies have demonstrated that multi-species biofilms are involved in periodontal disease progression rather than a single species infection (2). We found that patients with periodontal disease have a significantly higher number of detected species related to periodontal pathogens compared to healthy people. This data corroborates previous findings that periodontal disease is driven by polymicrobial infection (3). This data also suggests that pathogen-specific testing is insufficient to model the risk of periodontal disease progression, as dozens of strains may be uniquely involved in periodontal disease progression, further highlighting the utility of unbiased shotgun metagenomic sequencing in salivary diagnostics.
In this study we did not control for stage of periodontal disease, recent periodontal therapy, or symptoms of early gum disease like bleeding on probing or inflammatory markers. We expect that controlling for these factors will further improve algorithms to predict the progression of gum disease.