Our mouths are gateways to the rest of our bodies—so oral health plays a large role in reducing our risk for other diseases. The flip side of the coin is that oral disease can increase our risk for systemic diseases. Research shows how oral health status, specifically the mix of bacteria in our oral microbiome, influences our risk of diabetes or heart disease, as well as overall metabolic health. Now, growing research suggests that cognitive decline (including forms of Alzheimer's and other dementias) is connected to some of the same bacteria that cause gum disease.
The oral microbiome
Living inside our mouths are millions, even billions, of microbial neighbors: bacteria, fungi, and viruses. Many of these microbes have lived and evolved with humans over millions of years—what we call a "symbiotic relationship"—similar in some ways to how clownfish and anemones live together.
Some of these microbes are beneficial: they assist us with digesting food and fighting off disease. These are some of the same bacterial species you might find in your probiotics. Other bacteria, called "pathogens, "cause disease. One example you may be familiar with is Escherichia coli, otherwise known as E. coli. We all have commensal strains of E. coli living peacefully in our lower bowels. But unfamiliar strains can cause some serious digestive issues if they happen to be in your food. A few strains (e.g., E. coli O157:H7) can even produce toxins that lead to life-threatening illness.
Luckily, most microbes are either harmless or beneficial and only a small percentage are pathogenic. The type and abundance of pathogenic microbes in your personal microbiome influence your risk for disease. In a healthy mouth, the ecosystem of harmless and beneficial microbes keep the pathogens from growing out of control. Your oral microbiome is said to be in "dysbiosis" when the cumulative abundance of disease-causing microbes in your mouth passes a certain threshold and, like other infections, starts to provoke a reaction from your immune system.
Pathogenic microbes typically cause disease through one of two mechanisms of action:
The oral microbiome and oral health
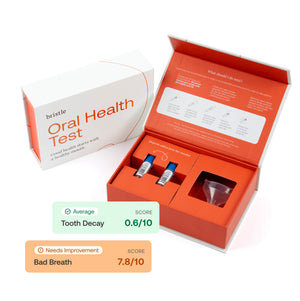
Bristle measures your oral health by analyzing the oral microbiome of a sample of your saliva. Typically, you have about 250 unique species of bacteria living in your mouth. Bristle’s technology enables us to identify all of them! To date, our microbiome analyses have identified over 700 different bacterial species that comprise the oral microbiota.

This illustration compares a healthy, balanced mouth, with an out-of-balance, dysbiotic, diseased one. The difference is the mix of microbes.
"Biogeography of oral microbiota colonization in the diverse habitats of the oral cavity." Lamont, R.J., Koo, H. & Hajishengallis, G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol 16, 745–759 (2018). https://doi.org/10.1038/s41579-018-0089-x
A subset of the 700 bacterial species in our mouths are pathogenic and can cause cavities, gum disease, and bad breath. By understanding the types and abundances of the bacteria in your saliva, Bristle can help you get insights into your oral health and risk for oral disease. We can suggest steps including hygiene, dietary, and lifestyle changes to eliminate pathogenic bacteria in your saliva - improving your oral health and lowering overall risk for disease.
The oral microbiome and overall health
For a long time, we've recognized connections between our oral and overall health, but new technologies allow us to understand better what drives them. For example, pathogenic microbes detected in our saliva that cause oral disease can make their way to other parts of our bodies, causing damage there as well. Improving your oral health through your oral microbiome can help improve your overall health and reduce your risk for disease.
Alzheimer's disease (AD)
Background
Alzheimer's disease (AD) is a form of dementia that affects memory, thinking and behavior. AD is the most common cause of dementia, producing some 60-80% of cases affecting an estimated 6M+ people in the US. AD is the sixth leading cause of death among Americans. Most patients are 65 or older and risk increases with age, although there are early-onset cases of AD. AD is a chronic and progressive neurodegenerative disease, meaning that the disease lasts for years, and worsens over time, eventually proving fatal if the patient doesn’t die of something else first. There are currently no cures, and only a handful of potential treatments are available. Therefore, an enormous amount of research is being conducted to find better ways of detecting, diagnosing, and treating AD.
How AD affects our brains
Our brains are made up of billions of interconnected nerve cells, called "neurons." Neurons behave like an integrated circuit board, sending and receiving information via neurotransmitter chemicals and electric signals that control all of our body's functions—basically biological programming. Groups of neurons can have special functions. Some are involved in helping us think, remember, and learn, while others focus on processing sight, smells, and sounds. These groups cluster in specific parts of the brain.
Our entire bodies are managed by nerve cells and, like car engines, they require a steady stream of fuel and oxygen to keep working well.
Scientists believe that AD starts with accumulating damage in groups of nerve cells, particularly those involved in learning, memory and orientation. Also like an engine, breakdowns in one part of the brain can cause damage in other parts, too. Nerve damage becomes more severe over time, resulting in increasing loss of function. Early symptoms include short-term memory loss (recent events are more likely to be forgotten than distant ones), but progress to wider memory loss, confusion, disorientation, mood and behavior changes and eventually, inability to walk, speak or swallow.
Current theories
The brains of patients with AD change drastically compared to patients without it, and a lot of research is focused on determining what changes cause AD and what changes are caused by it. Two prevailing suspects are in the lead as potential causes of nerve cell damage and death: plaques and tangles.
"Plaque" That sounds familiar—you've likely heard it from your dentist. Don't worry though, dental plaque—a sticky film produced by microbes in your oral microbiome—is different from plaque in your brain. In the case of AD, plaque refers to deposits of protein fragments that build up in the spaces between nerve cells.
"Tangles" are twisted fibers of certain proteins that build up inside nerve cells.
Plaque and amyloid-beta
Amyloid-beta proteins (AB) are small fragments of a larger protein called "amyloid precursor protein" (APP). AB is chemically stickier than other fragments of APP, meaning it is more likely to clump to form plaque. Plaque buildup is thought to disrupt cell functions like communication. Studies have shown that the brains of patients with AD have higher abundances of plaque. The major component of plaque formation comes from AB.
Three pieces of evidence are often cited for AB being a major factor in AD:
There are a variety of treatments being developed that target AB - attempting to slow down its production, remove it once it has formed, or prevent its formation altogether. But so far, none have succeeded in preventing neurodegeneration.
Tangles and Tau
Tangles, on the other hand, are proteins that become...well, tangled.
Our cells - including our neurons - are supported internally by structures called microtubules, similar to how houses are supported by beams and scaffolds. Microtubules also help transport nutrients into and within the cell.

In healthy cells, a protein called Tau binds to microtubules to help stabilize them. However, chemical changes can cause Tau molecules to detach from microtubules and stick to each other instead. This results in a "tangle" of Tau proteins that blocks nutrients from being transported inside the neuron and weakens the microtubules affecting the cell's structure. The damaged neuron is no longer able to communicate with other cells.
Realistically, Alzheimer's disease is driven by a variety of complex factors that are interconnected. Research shows that abnormal tau protein often accumulates in regions of the brain involved with memory. AB clumps in the spaces between neurons. As the levels of AB reach a tipping point, there is a rapid spread of tau throughout the brain.
Alternative theories
While AB, plaque, tangles and Tau remain the lead theories, the unhappy truth is that nearly 20 years of intense research has not shed much light on why and how AD develops. Nor has it led to any more than marginally successful drug treatments; most clinical trials have failed. So research is slowly pivoting to investigate alternative hypotheses.
Chronic inflammation
As we know from research into periodontal and autoimmune disease, chronic inflammation is bad news. Research now proposes that chronic neuroinflammation is a third key player, along with AB and Tau, in the development of AD. This may start with chronic activation of microglia, immune cells that normally keep the brain clear of waste and debris. Normally, such activation is in response to infectious microbes: bacteria or viruses. Microglia also activate in response to AB. At first, that’s healthy, as the microglia mop up AB molecules. But if there is too much AB, the microglia can’t keep up and begin to build up, along with stray molecules of AB. This may also trigger a build up of Tau tangles. Microglia also produce signaling chemicals (cytokines) that increase inflammation and can be toxic to neurons. Sometimes these processes continue in a harmful feedback loop, causing a chronic inflammatory response in the brain.
As with all complex biological diseases, your genes matter, too. In particular, TREM2 is a gene that tells microglia when it's time to clean up a cell. If it's not functioning properly, there will be a buildup of debris - including AB and damaged neurons. The immune system will call in another type of cell, an astrocyte, to clean up the resulting mess. But astrocytes, too, may become part of a cell and protein pile-up that eventually permanently destroys neurons.
Over time, the brain becomes crowded with microglia, astrocytes, damaged cells, stray protein molecules and plaque. The immune system will continue to launch attacks, further damaging the neurons it was meant to protect.
We already know that chronic inflammation in the gums is connected to systemic disease, adding to the likelihood of a connection between oral infection and AD.
Autoimmune connection
Chronic inflammation is a component of autoimmune disease as well. So it is not surprising that another theory about the causes of AD includes autoimmunity. In autoimmunity, immune system cells attack cells and tissue of their own host, confusing self antigens (chemicals that signal the identity of a cell) with antigens from pathogens. This confusion likely started with an infection by bacteria or viruses that have similar antigen patterns to host cells. A very large (n=1.8 million!) UK study found a significant correlation between hospitalization for certain autoimmune disease and later development of AD. Other research has suggested a link between herpes simplex virus (HSV) and AD. Yet other research is exploring autoantibodies and their connection to AD.
Blood vessel (vascular) conditions
While AD is considered the most prevalent dementia, vascular dementia is also common and may be confused with AD or Lewy body dementia. Primary vascular dementia is when damage to blood vessels through blockage (atherosclerosis) or bleeding (stroke) causes dementia symptoms. But vascular dementia may be combined with other causes.
However, chronic inflammation and plaque buildup can also affect our blood vessels, inhibiting the delivery of blood throughout our bodies. Our brains need blood—lots of it. Blood brings nutrients and oxygen to our brain passing through the blood-brain barrier, which protects our brains from harmful agents while passing through the nutrients and oxygen it needs.
Low blood flow reduces nutrients going to our brain and can damage the blood-brain barrier, which inhibits glucose from crossing into the brain and the clearing of plaque and debris out of the brain. This results in a build-up of amyloid-beta and tau proteins, chronic inflammation and the same bad feedback loop we discussed above.
Oral health and Alzheimer's
Background
Poor oral health has long been associated with cognitive decline. Research has shown correlations between tooth loss and dementia with a range of hypotheses attempting to explain the apparent link.
Like AD, the risk and prevalence of oral disease increases greatly with age. Both diseases are chronic, primarily affect US adults over 65 years old, and worsen over time. One theory is that missing teeth make chewing food more difficult, which results in nutritional deficiencies that can impact cognitive function. A study at NYU found that adults with more tooth loss had a 1.48x higher risk of developing cognitive impairment and 1.28x higher risk of being diagnosed with dementia, even after controlling for other factors. In fact, they found that each additional missing tooth was associated with a 1.4% increased risk of cognitive impairment and a 1.1% increased risk of being diagnosed with dementia.
“Given the staggering number of people diagnosed with Alzheimer’s disease and dementia each year, and the opportunity to improve oral health across the lifespan, it’s important to gain a deeper understanding of the connection between poor oral health and cognitive decline,” said Bei Wu, PhD, Dean's Professor in Global Health at NYU Rory Meyers College of Nursing, co-director of the NYU Aging Incubator, and senior author of this paper investigating the relationship between tooth loss and cognitive decline.
However, many studies to date have only correlated the occurrence of poor oral health and cognitive decline. New technologies are enabling a deeper view of the relationship between these two conditions.
Periodontal (gum) disease
Periodontitis, or gum disease, is a serious gum infection that damages the soft tissue and can destroy the bone that supports your teeth. Gum disease can cause teeth to loosen or lead to tooth loss. Periodontitis is common but largely preventable.
A subset of the microbes in your oral microbiome are pathogenic and can lead to periodontal disease. These microbes produce toxins that irritate our gums and stimulate a chronic inflammatory response, which can cause the tissue and bone that support our teeth to break down. Gums separate from the teeth, forming pockets (spaces between the teeth and gums) that become even more infected.
Gum disease progresses in stages, from the mildest form (gingivitis) to more severe stages. Once it advances to a certain point it becomes chronic and irreversible - requiring regular treatments and procedures to manage symptoms.

Gum disease is EXTREMELY common and affects an estimated 47% of US adults - over 60M people. It is most common in adults over the age of 50 and becomes more prevalent with age - 70% of adults over 65 years old have gum disease.
Gum disease is a major cause of tooth loss, which as we've discussed, is associated with cognitive decline, making gum disease a major area of interest in understanding the emergence and progression of Alzheimer's.
Studies have found correlations between periodontal disease and Alzheimer's. One hypothesis is that the pathogenic bacteria associated with gum disease travel outside of our mouths by entering the bloodstream, causing systemic inflammation that can lead to a variety of disorders including cancer, diabetes, and cardiovascular and neurological diseases.
There are a number of ways pathogenic bacteria from our mouths can get into our bloodstream. Micro-injuries are one: while we're flossing, brushing, chewing certain foods, or during dental procedures like root canals and tooth extractions.
Periodontitis and AD often coexist. However, research is focused on answering a key question: which comes first? Some studies have demonstrated that people with periodontitis present a major risk of developing AD while others suggest that those with AD or dementia have poor oral hygiene habits stemming from cognitive decline, and therefore are more likely to develop gum disease. These may both be true, but it’s easier to prevent and treat periodontitis early than wait until dementia symptoms emerge.
P. gingivalis
There are over 700 characterized types of bacteria known to be in the oral microbiome, and on average we each live with around 250 in our mouths. One of these species, Porphyromonas gingivalis (P. gingivalis), is among the most well-characterized. Why is there so much interest in this single species?
Well, have you ever heard of "gingivitis"? Now you know where the name comes from! P. gingivalis is an infamous bacteria associated with the emergence and progression of gum disease. You might see it in your Bristle oral health insights. A study in 2008 showed P. gingivalis was present in over 85% of samples from patients with chronic periodontitis.
P. gingivalis is:
non-motile, asaccharolytic, Gram-negative bacterium, an obligately anaerobic rod which forms black-pigmented colonies on blood agar plates
Translated into language we can all understand:
Non-motile: lacks the structures that enable free movement. This makes perfect sense given that P. gingivalis lives in dental plaque!
Asaccharolytic: incapable of breaking down carbohydrates (like sugar) for energy. Why is this relevant? P. gingivalis lives below the gum-line, where access to sugar is low. If P. gingivalis relied on sugars to survive, then it would starve. Instead, P. gingivalis processes amino acids, the building blocks of proteins, which are more readily available. Bacteria associated with cavities, on the other hand, tend to live on the surface of teeth, where there is more access to sugar. As expected, these bacteria feed on carbohydrates and convert them into acids, which lead to decay.
Gram-negative: Gram-staining is a method used to differentiate types of bacteria into two large groups (positive and negative). Gram-negative bacteria have a fat+sugar coating (lipopolysaccharide) on their cells which resists the violet Gram-stain. Gram-positive bacteria, lacking this coat, take up the dye and turn violet. . Gram-negative bacteria tend to be more resistant to antibiotics and other therapeutics, in large part because of their lipopolysaccharide coats.

Anaerobic: survives and grows in areas that lack oxygen. Obligate means they only survive in the absence of oxygen. This is an important characteristic for P. gingivalis since oxygen is absent beneath our gum line. Oxygen destroys anaerobes, which is a big part of why flossing is so important!
So P. gingivalis doesn't move on its own, it doesn't feed on carbohydrates, it is resistant to many antibiotics and therapeutics, and it thrives in areas that lack oxygen. All of these factors make it the perfect candidate for infiltrating our gums and causing disease.
P. gingivalis produces direct and indirect mechanisms that lead to gum disease.
P. gingivalis and Alzheimer's - the gingipain hypothesis
P. gingivalis has been identified in the brains of patients diagnosed with Alzheimer's, which may not come as a surprise given the correlation between poor oral health and cognitive decline.
Gingipains—a family of toxins produced by P. gingivalis—have drawn the majority of attention from researchers investigating oral health and cognitive decline. A landmark study uncovered a correlation between the levels of gingipains and amyloid-beta / tau protein levels in the brains of patients with AD. The researchers also identified P. gingivalis in the brains and cerebrospinal fluid (CSF) of those same patients. In fact, further research showed that gingipains were found in neurons of over 90% of patients' brains diagnosed with AD.
The study suggests that P. gingivalis can migrate from the oral cavity into the bloodstream, eventually making its way to the brain. Once there, P. gingivalis produces gingipains, which are associated with increased levels of amyloid-beta and tau proteins, eventually leading to cognitive decline.
Our identification of gingipain antigens in the brains of individuals with AD and also with AD pathology but no diagnosis of dementia argues that brain infection with P. gingivalis is not a result of poor dental care following the onset of dementia or a consequence of late-stage disease, but is an early event that can explain the pathology found in middle-aged individuals before cognitive decline. We also demonstrate that P. gingivalis bacterial load can be detected in the CSF of clinical AD patients, providing further evidence of P. gingivalis infection of the CNS... Although not specifically addressed in this report, once the oral cavity is infected, P. gingivalis may access the brain and spread via a number of pathways...After entering the brain, we suggest that P. gingivalis may spread slowly over many years from neuron to neuron
How are gingipains related to amyloid-beta and tau?
Let's do a quick recap on what we've learned so far:
Amyloid-beta (AB) and tau are two proteins that are thought to play a key role in the formation and progression of AD. Increased levels of each are found in the brains of patients diagnosed with AD and are thought to form plaques and tangles that may lead to neuron damage associated with cognitive decline. AB is found in the spaces between neurons, whereas tau is found inside the neurons themselves.
Poor oral health has long been associated with cognitive decline. Similar to AD, the risk and prevalence of oral disease and tooth loss increases steeply with age. In particular, gum disease has been a key area of interest due to its link with chronic inflammation, which is thought to also play a role in AD. We know that pathogenic bacteria involved in gum disease are implicated in other systemic inflammatory conditions including diabetes and heart disease by way of these bacteria entering our bloodstreams.
While there are a variety of microbes that trigger gum disease, P. gingivalis is the most infamous and well-characterized species. Studies have identified P. gingivalis in the brains and cerebrospinal fluid of patients diagnosed with AD. One toxin specifically produced by P. gingivalis, gingipains, has also been found in the brains of patients diagnosed with AD at levels that correlate with AB and tau increases.
Amyloid-beta: friend or foe (or both)?
Contrary to what you might believe based on what we've discussed so far, some studies have suggested that amyloid-beta is normally beneficial! Amyloid-beta is found across all humans and throughout our lives. Researchers believe AB plays a key role in protecting the body from infections, repairing leaks in the blood-brain barrier, promoting recovery from injury, and regulating synaptic function.
So how does something that should be helpful end up harming us? Like everything else in health and biology: context and moderation are key.
Amyloid-beta has shown antibacterial, antifungal, and antiviral properties effective against several species of microbes. When we are infected by these microbes, our bodies increase the production of amyloid-beta to combat them. While more infection-fighting AB sounds like a good thing, it also increases the chance for error in production. Errors in AB can lead to loss of function—it may be less effective in fighting off an infection or may take longer to clear out from our bodies. If we accumulate malfunctioning AB, effects may be more severe and the infection it was supposed to protect us from may actually get worse.
Evidence from our work reported here lends support to the emerging concept that Aβ is an antimicrobial peptide, and mutations contributing to loss of this function could allow more robust infection with P. gingivalis and higher risk for disease. In addition, sustained high levels of antimicrobial Aβ driven by chronic P. gingivalis infection of the brain may be toxic to host cells...
How it all fits together
What's being done today?
Deeper insights into the drivers and mechanisms of disease provide opportunities to create more effective therapeutics and treatments against them. While there are a variety of companies and researchers investigating new ways to detect and treat cognitive decline, we wanted to highlight two exciting companies in this space, as it relates to P. gingivalis and Alzheimer's.
*Bristle does not have any personal or professional relationships with the companies cited below!

An example of how P. gingivalis may contribute to the onset and progression of cognitive decline.
Cortexyme
Cortexyme is a clinical stage pharmaceutical company based in South San Francisco, CA, focused on creating new therapeutics to improve the lives of patients diagnosed with Alzheimer's and other cognitive diseases.
Their lead therapeutic candidate is a small-molecule called atuzaginstat (COR388) which is being tested for treating patients with mild to moderate Alzheimer’s disease. COR388 is a "novel virulence factor inhibitor" targeting gingipains from P. gingivalis. What does that mean?
Source: https://vimeo.com/333736696
It means that COR388 is intended to "inactivate" the gingipains that are produced by P. gingivalis and stop or slow down damage to healthy brain cells by reducing or eliminating their effect on amyloid-beta and tau production.
They are currently conducting a large-scale clinical trial—the GAIN Trial—which has shown some exciting initial data. Interestingly, Cortexyme included a sub-study (REPAIR) to analyze COR388 and another compound, COR588, in treating and preventing periodontal disease. Both molecules have been shown to penetrate oral biofilm and target P. gingivalis while it's still in the oral cavity—something that is traditionally difficult to do since P. gingivalis is a gram-negative species of bacteria*.*
Cortexyme's CEO, Casey Lynch, said:
Cortexyme is in a unique position with a pivotal clinical study of our lead drug candidate atuzaginstat that targets the infectious pathogen P. gingivalis not only as the causative agent of Alzheimer’s disease, but also its well-established role as a keystone bacterium for periodontal disease. This presents us with the potential to provide innovative and breakthrough treatments in two high unmet clinical need areas with a first-in-class, orally administered small molecule,
You can find a list of their publications and citations here.
Keystone Bio
Keystone Bio is another company leveraging the connection between oral health and cognitive decline to develop new therapeutics. Their website describes their approach:
Using KB [Keystone Bio] proprietary methods, KB has discovered a bacterial toxic protein that is a primary driver of systemic inflammation. This bacterial toxic protein complex is secreted actively in large amounts by the bacteria for its own survival, however it has off-site systemic pathology in various end organs such as the brain in AD brain tissues. This virulent protein complex is packaged into distinct outer membrane vesicles, breaking down and crossing the BBB, and impacts the brain parenchyma in specific neuro-anatomic locations consistent with AD development.
Keystone Bio is also targeting P. gingivalis through a variety of therapeutic candidates. Their lead candidate, KB-001, is a monoclonal antibody that selectively binds to P. gingivalis preventing it from colonizing in the oral cavity. Lowering the abundance of P. gingivalis should impact the downstream accumulation of gingipains. If the hypothesis is correct, this should reduce the buildup of amyloid-beta and tau proteins in the brain.
Why the name "Keystone Bio?" The company is named for their central hypothesis - that p. gingivalis is a keystone pathogen. The term "keystone pathogen" refers to the hypothesis that there are certain microbes, even at low abundances that can orchestrate a severe inflammatory response by catalyzing dysbiosis in an otherwise healthy microbiome.
Final thoughts
Long-known correlations between poor oral health and cognitive decline, and new research studies suggest that gum disease may contribute to and progress Alzheimer's disease. One pathogenic bacteria, P. gingivalis, has characteristics and a growing body of evidence that make it the primary suspect linking these two conditions.
Today's research and data suggest a few important ideas:
Our oral and cognitive health are closely linked—we've seen evidence of associations between oral disease and systemic conditions including diabetes, heart disease, and Alzheimer's.
Improving oral health and preventing oral disease may reduce our risk or prevent systemic disease in the future.
A word to the wise
As with all emerging research, we encourage you to keep in mind that these studies and their results are not deterministic. We are only just beginning to understand the role of oral health and the oral microbiome in our overall health. Today's evidence does not prove beyond a doubt that P. gingivalis or gum disease directly causes Alzheimer's disease. Do not interpret the information in this article or in the papers we cite as medical or dental advice.
With that said, it is a fact that good oral health is (at the very least) an important component of good overall health. We encourage all of you to take steps toward improving your oral health and minimizing the risk for oral disease. If these hypotheses prove to be correct, then that means addressing your oral health may reduce or eliminate cognitive decline, and possibly reduce your risk for other systemic diseases too!
At Bristle, we believe that addressing and improving your oral health is one of the most essential and actionable steps in improving overall health. Through our tests and insights, we provide everyone with the tools they need to improve their oral health. Lots of small improvements can create a massively positive impact — and we think that your mouth is a pretty great place to start.
Citations
Oral health & microbiome
Oral microbiome and health
Insights into the human oral microbiome
Impact of systemic factors in shaping the periodontal microbiome
The Oral Microbiome in Health and Its Implication in Oral and Systemic Diseases
Oral microbiome: Unveiling the fundamentals
The oral microbiota – a mechanistic role for systemic diseases
sj.bdj.2018.217.pdf
Oral health & heart disease
Mediators between oral dysbiosis and cardiovascular diseases
Cardiovascular disease and the role of oral bacteria
Nitrate, the oral microbiome, and cardiovascular health: a systematic literature review of human and animal studies
Gut microbiota and cardiovascular disease: opportunities and challenges
The human microbiota is associated with cardiometabolic risk across the epidemiologic transition
Oral health & diabetes
Diabetes and oral health - NIDCR
Oral Microbiome Signatures in Diabetes Mellitus and Periodontal Disease
Association of the oral microbiome with the progression of impaired fasting glucose in a Chinese elderly population
Oral & metabolic health
Microbiota and metabolic diseases
Alzheimer's disease
What is Alzheimer’s Disease?
What Is Dementia? - CDC
What is Dementia? - Alzheimer's Association
Dementia vs. Alzheimer’s Disease: What is the Difference?
Research & Progress
Inside the Brain
Amyloid-Beta and Tau
What Happens to the Brain in Alzheimer's Disease?
Amyloid-β and Tau in Alzheimer's Disease: Novel Pathomechanisms and Non-Pharmacological Treatment Strategies
Amyloid-β and tau: the trigger and bullet in Alzheimer disease pathogenesis
Synergy between amyloid-β and tau in Alzheimer’s disease
Beta-amyloid and the amyloid hypothesis
Beta-amyloid and the amyloid hypothesis.pdf
Tau
Tau.pdf
Oral health and Alzheimer's
Background
Poor oral health conditions and cognitive decline: Studies in humans and rats
Tooth Loss Associated with Increased Cognitive Impairment, Dementia
Dose-Response Meta-Analysis on Tooth Loss With the Risk of Cognitive Impairment and Dementia
Poor oral health linked to cognitive decline, perceived stress
U.S. state correlations between oral health metrics and Alzheimer’s disease mortality, prevalence and subjective cognitive decline prevalence
Periodontal disease
Oral microbiota of periodontal health and disease and their changes after nonsurgical periodontal therapy
The Oral Microbiome in Periodontal Health
The oralome and its dysbiosis: New insights into oral microbiome-host interactions
Types of gum disease
Periodontal Disease
Periodontal Disease in Adults (Age 30 or Older)
P. gingivalis
Porphyromonas gingivalis: An Overview of Periodontopathic Pathogen below the Gum Line
Human variation in gingival inflammation
The cell biology of bone metabolism
Oral microbiome and Alzheimer's
Oral microbiota and Alzheimer’s disease: Do all roads lead to Rome?
The Oral-Gut-Brain AXIS: The Influence of Microbes in Alzheimer’s Disease
Is There Any Association Between Neurodegenerative Diseases and Periodontitis? A Systematic Review
Large study links gum disease with dementia
Porphyromonas gingivalis and Alzheimer disease: Recent findings and potential therapies
Clinical and Bacterial Markers of Periodontitis and Their Association with Incident All-Cause and Alzheimer's Disease Dementia in a Large National Survey
Gingipain hypothesis
An update and baseline data from the Phase 2/3 GAIN trial of COR388 (atuzaginstat) a novel bacterial virulence factor inhibitor for the treatment of Alzheimer’s Disease
Porphyromonas gingivalis Gingipains and Adhesion to Epithelial Cells
Porphyromonas gingivalis Outer Membrane Vesicles as the Major Driver of and Explanation for Neuropathogenesis, the Cholinergic Hypothesis, Iron Dyshomeostasis, and Salivary Lactoferrin in Alzheimer’s Disease
Periodontal dysbiosis associates with reduced CSF Aβ42 in cognitively normal elderly
Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors
Alzheimer's Disease-Like Neurodegeneration in Porphyromonas gingivalis Infected Neurons with Persistent Expression of Active Gingipains