Bristle research digests are short research articles that share some of the insights around the oral microbiome and how it impacts health and disease. All data come from Bristle’s internal research, which leverages the Bristle Comprehensive Oral Microbiome Test, a saliva-based at-home test that measures microbes in the oral microbiome using shotgun metagenomic sequencing.
*this article was updated June 14,2022 with new plots to add statistics between some groups (by wilcoxon rank sums).
Flossing and oral health
There is a widely established understanding that good oral hygiene reduces your risk of developing tooth and gum disease. While brushing is a key component of this, one of the most important parts of a comprehensive oral hygiene regimen is flossing. We’ve all been taught that daily flossing is critical to keeping our mouths healthy, but surprisingly, the breadth of data supporting this recommendation is lacking.
A systematic review of 12 randomized control trials, published in the Cochrane Database of Systemic Reviews in 2011, which compared flossing + toothbrushing versus toothbrushing alone showed weak and unreliable evidence to suggest that the addition of flossing to toothbrushing may be associated with a small reduction in plaque at 1 or 3 months.
Given this weak association and discrepancy in what is routinely taught, we decided to directly study the impact of flossing ourselves.
Background
The Bristle Comprehensive Oral Microbiome test analyzes the oral microbiome by measuring the relative abundance of over 30,000 bacterial strains. Using the oral microbiome, Bristle has developed scores for gum inflammation, tooth decay, and halitosis. Here we share a number of our research findings through analyzing the oral microbiome with lifestyle, hygiene, and other data to provide data-driven recommendations on how you can improve your health.
The study
We asked 100 Bristle users who also took a Bristle test about their oral hygiene habits. At Bristle, we use several internally developed algorithms for gum disease, dental caries, halitosis, and commensal bacteria among others as surrogates for disease and health.
Results
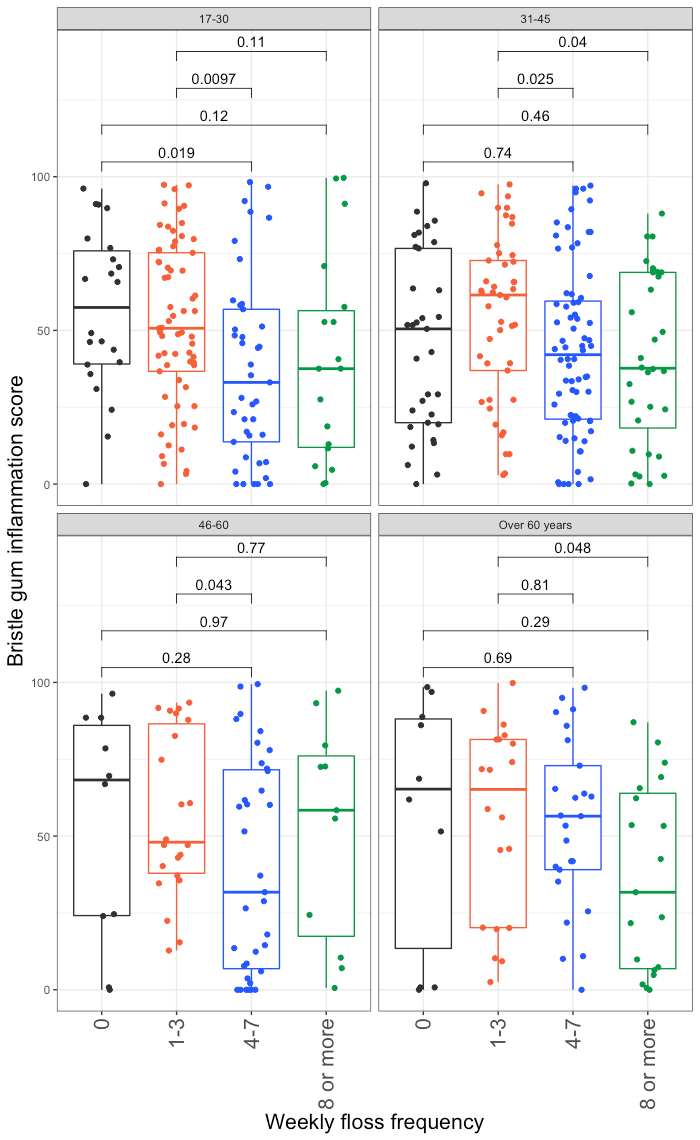
Note❗ For all of the graphs below: Each dot represents the microbiome scores calculated from a single saliva sample from a different Bristle user. The box plots show the 25th, 50th, and 75th quantiles for each group. The y axis from each plot shows a different Bristle score, and the x-axis shows self-reported flossing frequency. The dots are jittered for easier visualization.
We found that the frequency of flossing is highly correlated to scores for gum disease, halitosis, and tooth decay. Users who reported not flossing at all had an average gum inflammation score of 70.65, while flossing even just 1-3 times per week significantly reduced scores to an average of 58.67. Flossing 4-7 or 8 or more times per week further reduced gum inflammation scores to 53.08 and 44.23 respectively. A similar trend was seen with halitosis, and tooth decay scores, although flossing frequency more than 4-7 times per week did not improve halitosis or tooth decay scores. Unsurprisingly, we found that flossing frequently was positively correlated with an increase in commensal scores. Commensal scores are driven by the abundance of species that are unrelated to disease and potentially beneficial, and this increase is driven partially by the decrease in the species related to disease. These commensal species also play a larger role in the community by creating antimicrobial peptides such as bacteriocins that prevent pathogenic species from colonizing.




As a control, we looked at the relative abundance of Neisseria, Actinomyces and Streptococcus, three genuses we would not expect to be broadly affected by flossing frequency. In two cases, we did not find a strong correlation with flossing and their relative abundance. However, the relative abundance of Actinomyces species significantly decreased with flossing frequency, possibly because Actinomyces thrive under anaerobic conditions.



Furthermore, we looked at whether age was a major factor driving the trends with flossing frequency, but found that flossing frequency was evenly distributed among age groups, and broadly the correlations between gum inflammation scores, commensal scores, and flossing frequency held true regardless of age with a few exceptions that we are currently investigating.

Finally, we looked at whether existing periodontal disease had an affect on the trends we saw or with flossing frequency. We found that even in patients with irreversible periodontal disease (characterized by ≥5mm pocket depth and irreversible bone loss), flossing frequency was still still correlated with a reduction in gum disease scores. In general, as expected, patients without periodontal disease had much lower scores, and thus saw less absolute improvement in their scores. More samples are needed to make conclusions about this data.

Conclusions
Flossing frequency is highly correlated with a reduction in gum inflammation scores, halitosis scores, and caries scores. The reduction in gum and halitosis scores is likely driven by a reduction in the relative abundance of anaerobes that drive their respective diseases. We speculate that the correlation of flossing with caries may be due to a decrease in the acidogenic microbes that colonize between teeth and cause interdental caries. In general, flossing 1-3 times per week is insufficient to drive significant oral microbiome change, and the most benefit came from flossing roughly once per day, with marginal improvement at best when flossing multiple times per day.
One caveat to these findings is that users who floss more frequently may generally take better care of their oral health, and partake in other behaviors that may influence their oral microbiome.