Gingivitis is the medical term for inflamed gums. Almost half (46%) of US adults over age 30 have some form of gum disease. With the accessibility and affordability of modern dental care, this statistic might be surprising.
However, it is all too easy to disrupt the balance of the good and bad bacteria that live in your mouth, which is one reason why gingivitis is so common. Even more, gum disease often comes silently--unnoticed by those who have it until serious symptoms develop.
Here’s what you need to know to help protect your gums. Gums are as important a part of your oral health as your teeth!
Gingivitis vs periodontitis
What is gingivitis? Also known as gum disease, gingivitis is a mild form of periodontitis. It is inflammation of the gums, which may or may not be painful. Severe gum disease, called periodontitis involves not only inflammation, but infection under the gums of deeper tissues, which can lead to tooth damage and eventually tooth loss if left untreated.
Gingivitis is milder, but is often a precursor to more serious problems, like periodontitis, so take note! Your body is trying to tell you something.
What causes gum disease?
Let’s be honest here. Most gum disease is completely preventable by you, it’s just a matter of keeping up with your dental hygiene.
Why?
Your mouth is full of bacteria, (think about that the next time you want to kiss somebody!). There are both good and bad species of bacteria living in your mouth. When the bad grows to crowd out the good, boom! You end up with gingivitis (or cavities).
Every day, sugars and starches in foods you eat feed the bad bacteria in your mouth, which form plaque. This sticky biofilm adheres to your teeth and eventually turns into hard tartar if not removed daily. The tartar creates a protective shield for bad bacteria to live and grow happily while they begin to destroy your teeth.
This buildup of tartar and plaque on teeth irritates the gums, leading to gingivitis.
Your risk of developing gingivitis is influenced by many factors. These include:
Gingivitis symptoms to look out for
How do you know if you have gingivitis? Your gums may look a bit (or a lot) red and puffy--that’s inflammation. They may be tender or painful to touch. They may bleed easily when you brush or floss your teeth. As gingivitis progresses, your gums may form visible pockets. You (or the people around you) also may notice bad breath.
Eventually, your gums may begin to recede, exposing tooth roots. If you wait long enough, your teeth may begin to loosen.
How gum disease affects the rest of the body
While inflamed gums and tooth loss are bad enough, gum disease can affect the rest of your body. Researchers have been discovering links between gum disease and various systemic diseases such as cardiovascular disease, cancer, diabetes, and even Alzheimer’s disease! Since these rank among the leading causes of death in the US, it’s something to pay attention to. Autoimmune diseases, too, like rheumatoid arthritis, have been linked to diseased gums.
How can problems in your mouth have such an effect on the rest of your body? Bad bacteria can enter your bloodstream through tiny cuts in your irritated gums (sometimes called leaky gums). Once loose, they may infect distant parts of the body (like heart valves or joints). Or they can release chemicals that trigger inflammation or an immune response..
Easy ways to prevent gum disease
The good news is that there are plenty of things you can do to stop and even reverse gum disease. Learn how to get rid of gingivitis here.
Practice regular oral hygiene
Most of all, brush and floss your teeth every day. It really is that simple. Plaque and tartar on your teeth give bad bacteria a place to hang out. Remove plaque regularly and they don’t have a home.
If you notice that your gums look a little swollen or bleed easily, step up your oral healthcare routine. Rinse, brush and floss after every meal rather than once a day. But be gentle, brushing or flossing too hard is not cleaning better.
Try an electric toothbrush
If you don’t already use one, you might consider switching to an electric toothbrush. Electric toothbrushes are more effective at removing plaque and helping to reduce the occurrence of gingivitis. They are also more gentle than hand brushing.
Add mouthwash
Another option is to start using mouthwash in addition to brushing and flossing. An antiseptic mouthwash can help kill the bad bacteria living in your mouth. Dry mouth can exacerbate problems with bacteria, so choose an alcohol-free variety of mouthwash if you already suffer from dry mouth.
Visit the dentist
You can also visit your dentist for a deep cleaning. Over time, plaque turns into tartar, a hard substance that is difficult to remove from your teeth with brushing and flossing alone. However, a dental professional can remove it with special tools. She can also see the plaque more easily than you can in a mirror. The dentist can also tell you how advanced your gum disease is by measuring gum pockets.
Many times, regular dental cleaning is sufficient. If the situation is bad enough, dentists may perform a procedure called scaling and root planing. This involves scraping plaque and tartar off the teeth (including under the gums). The teeth are then smoothed (planing) to encourage the gums to reattach to them as well as discourage the growth of new plaque.
Do you have gingivitis?
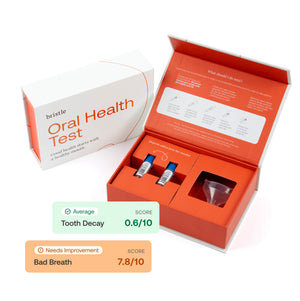
Do you suspect you have gingivitis? You can find out without having to visit an in-person dentist through our unique service.
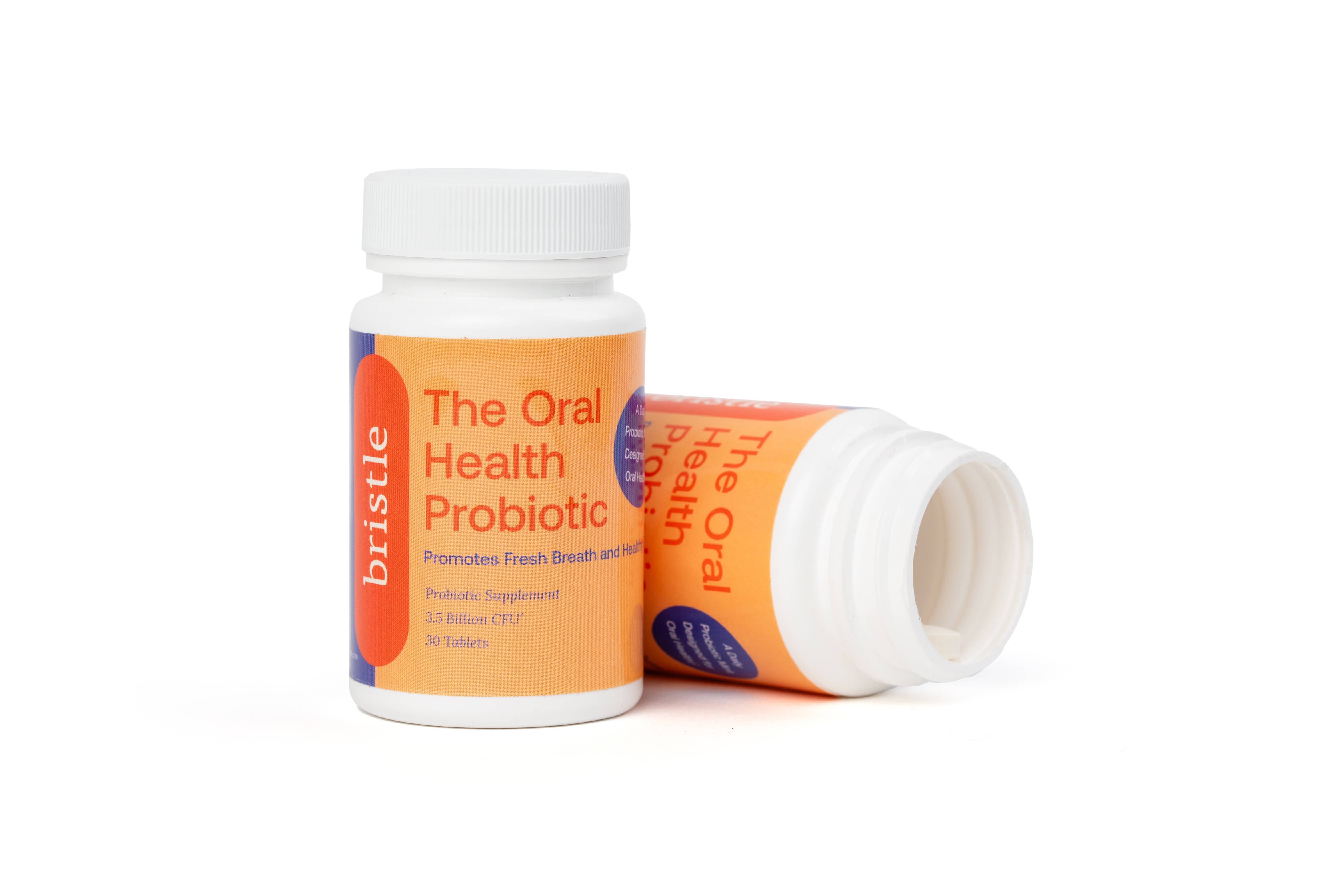
Send us a saliva sample and we’ll tell you what kinds of bacteria are thriving in your mouth and if gingivitis — or any other issues — are something you should worry about. Armed with this knowledge, you can learn how to treat gingivitis and begin at-home treatments to combat these issues and restore a healthy balance of bacteria in your mouth.
Check it out today!