In this article, we’ll explore the meaning of oral microbiome dysbiosis, how the oral microbiome impacts oral health and overall health, and ways to fix oral microbiome dysbiosis.
What is the oral microbiome?
The oral cavity hosts a a variety of ecological niches, places where microbes can survive and grow. The microbial composition in the oral cavity is known as the oral microbiome. The majority of microbes in the oral microbiome are bacteria. These bacteria live on your teeth, between your teeth and gums, on your tongue, your cheeks, and all over your mouth. These microbes are part of a community of microbes, called the oral microbiome, and the bacterial composition determines the majority of the oral microbiome.
The different environments in the mouth allow for different types of microbial communities to grow. For instance, the front of your tongue primarily hosts aerobic bacteria, ones that are great at surviving in the presence of oxygen. In contrast, the bacteria that live at your gum line are mostly anaerobic or microaerophilic, meaning they can only survive in low levels of oxygen or in the complete absence of oxygen.
The microbes that live throughout your mouth provide health benefits, through creating metabolites that support your health, to priming and training your immune system. This symbiotic relationship continues under normal healthy conditions. The bacteria that support health and homeostasis are called the commensal microbiota. But if the wrong ones are growing, microbes can also cause disease and wreak havoc on your mouth, and even the rest of your body. Harmful bacteria that live in your mouth can trigger inflammation, and cause infections. This condition where harmful microbes can grow and cause disease is due to microbial imbalance in the community, also known as dysbiosis.
Your oral microbiome is like a garden, it requires constant maintenance to keep the plants in the garden alive and healthy. If these plants begin to die, its more likely for weeds to come and take their place. The oral microbiome is in a constant state of balance, and sometimes weeds come along and cause imbalance.
What is oral microbiome dysbiosis?
Oral microbiome dysbiosis is a condition where there is an imbalance of beneficial and harmful microbes in the mouth. The microbiome in health, the harmful microbes are kept at low abundance by the beneficial microbes and your immune system.
However, in conditions where beneficial microbes become reduced, or ecological niches are empty, this allows for harmful bacteria to grow into the space, trigger an immune response, and cause disease. This often happens after someone takes antibiotics, and the microbiome is wiped out and the ones that take hold are often opportunistic pathogens that thrive when nothing else in the microbial communities can keep it in check.
Similar to an empty garden, weeds and invasive plants are able to easily grow. However, if a garden is packed full of flowers, shrubs, and trees, there is little space and nutrients remaining for weeds to use to grow. The oral microbiome is a similar ecosystem.
What diseases are caused by oral microbiome dysbiosis?
The most common oral diseases are cavities and gum disease, both are associated with oral microbiome dysbiosis.
Cavities and the oral microbiome
Cavities are caused by acid producing bacteria that ferment the excess sugars in your mouth and saliva. This acid leads to tooth decay, which erodes enamel. These bacteria reduce the overall pH at the surface of teeth and your mouth, which leads to dysbiosis. Acid-resistant bacteria then outcompete the normal healthy microbiome, causing more cavities and oral disease.
Fortunately, commensal symbiotic bacteria can increase the pH of your mouth, especially through a pathway called arginine deiminase pathway. Arginine is metabolized by these helpful species, creating ammonia ions that increase the pH, neutralize acid, and aid in teeth remineralization. The microbiome in health supports the remineralization of enamel, while dysbiosis contributes to decay and demineralization.
Gum disease and dysbiosis
Gum disease is cause by specific anaerobic bacteria that live at the gumline, between your teeth and gums, and cause inflammation. These pathogens are normally kept at low abundance in the oral microbiome. However, when the balance shifts, healthy commensal bacteria in the oral microbiome are no longer able to maintain the pathogenic ones in check. Additionally, your immune system is unable to keep up with the pathogenic bacteria, leading to dysbiosis.
Gum disease is a polymicrobial infection, meaning it is caused my multiple bacterial species rather than a single type of bacteria. These pathogenic species work together to invade tissue, leading to an inflammatory response. Chronic inflammation can even lead to damage of the bone and periodontal disease. By contrast, commensal healthy bacteria also work together to maintain homeostasis.
For example, Treponema denticola and Porphyromonas gingivalis, two gum disease pathogens, interact to grow more quickly and invade gum tissue. When healthy, these pathogenic species are independently kept at low levels. Together, they create molecules and proteins that synergize and can inhibit your immune system to worsen dysbiosis.
Bad breath and dysbiosis
Chronic bad breath is a sign of oral dysbiosis, and may be an early indicator of gum disease. Porphyromonas gingivalis and other periodontal pathogens are anaerobes that create foul smelling compounds, called volatile sulfur compounds.
Research also shows that specific bacteria that do not typically cause gum disease, like Solobacterium moorei, Granulicatella adiacens, Klebsiella, and Enterobacter species can also cause bad breath. These species are much higher in people with oral microbiome dysbiosis. Under healthy conditions, these species are unable to grow to high abundances because commensal species keep them low.
Oral thrush
Candidiasis, or infection by the opportunistic pathogen yeast Candida, is incredibly common. Most people have Candida in their oral, fecal, and skin microbiome at low abundance. However, in cases where the immune system is weakened, Candida can rapidly grow, and at high abundance causes the disease thrush. Research is still being done to understand the complex dynamics between yeast and bacteria in the oral microbiome, but studies have shown distinct oral microbiome profiles in people with chronic and recurring thrush.
Systemic health and the oral microbiome
Research has shown numerous links between overall health and the oral microbiome. Here are just a few examples of those associations with systemic diseases:
Cancer
For example, some cancers such as colon cancer, oral cancer, and pancreatic cancer, are associated with the higher bacterial abundance in the mouth such as Porphyromonas gingivalis and Fusobacterium nucleatum. These species have been shown to promote tumor progression, potentially through triggering chronic inflammation that exacerbates disease. Importantly, the increased abundance of these species is also a signature of oral microbiome dysbiosis.
Cognitive decline and neurological disease
The oral microbiome is also associated with conditions related to cognition and the brain. For example, P gingivalis has been found in the brains of people with Alzheimer’s disease, demonstrating a clear link between the mouth and the brain, also known as the oral-brain axis.
Diabetes
The oral microbiome has been shown to change dramatically in people with diabetes. People with diabetes have higher levels of sugar in their saliva, which causes oral microbiome dysbiosis, as it allows microbes to more easily propagate in the mouth. Specific changes to the oral microbiome have been identified in people with diabetes.
Heart disease
Bacterial species such as Treponema denticola and Porphyromonas gingivalis, and Fusobacterium nucleatum are all key species that have been shown to affect risk of heart disease and cardiovascular disease. These bacteria have even been found inside atherosclerotic plaque, the accumulation of cholesterol and fat that clogs arteries.
How can I fix oral microbiome dysbiosis?
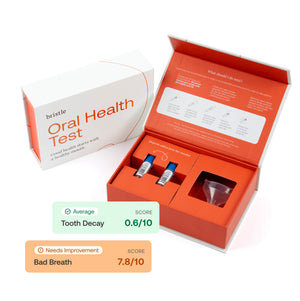
Research has demonstrated that a few diet, lifestyle, and hygiene changes may be helpful in reverting oral microbiome dysbiosis back to a balance state. However, knowing your oral microbiome status with an oral microbiome test is the first step. You can’t know which direction to step if you don’t know what your starting point is!
Xylitol
Xylitol is easy to add to your oral hygiene regimen as a chew, lozenge, or rinse, and can prevent fermentation by S. mutans and other cavities causing bacteria that create acid.
Arginine
Arginine is a prebiotic amino acid that modulates the oral microbiome by enriching for alkali-generating commensal bacteria that increase local pH, prevent enamel demineralization, and improve remineralization of teeth.
Nitrate
Nitrate is a prebiotic molecule that has been shown to enrich for aerobic commensal bacteria, and decrease anaerobes that cause disease. Eating foods high in nitrate are correlated with improved oral health, cognitive, and cardiovascular health.
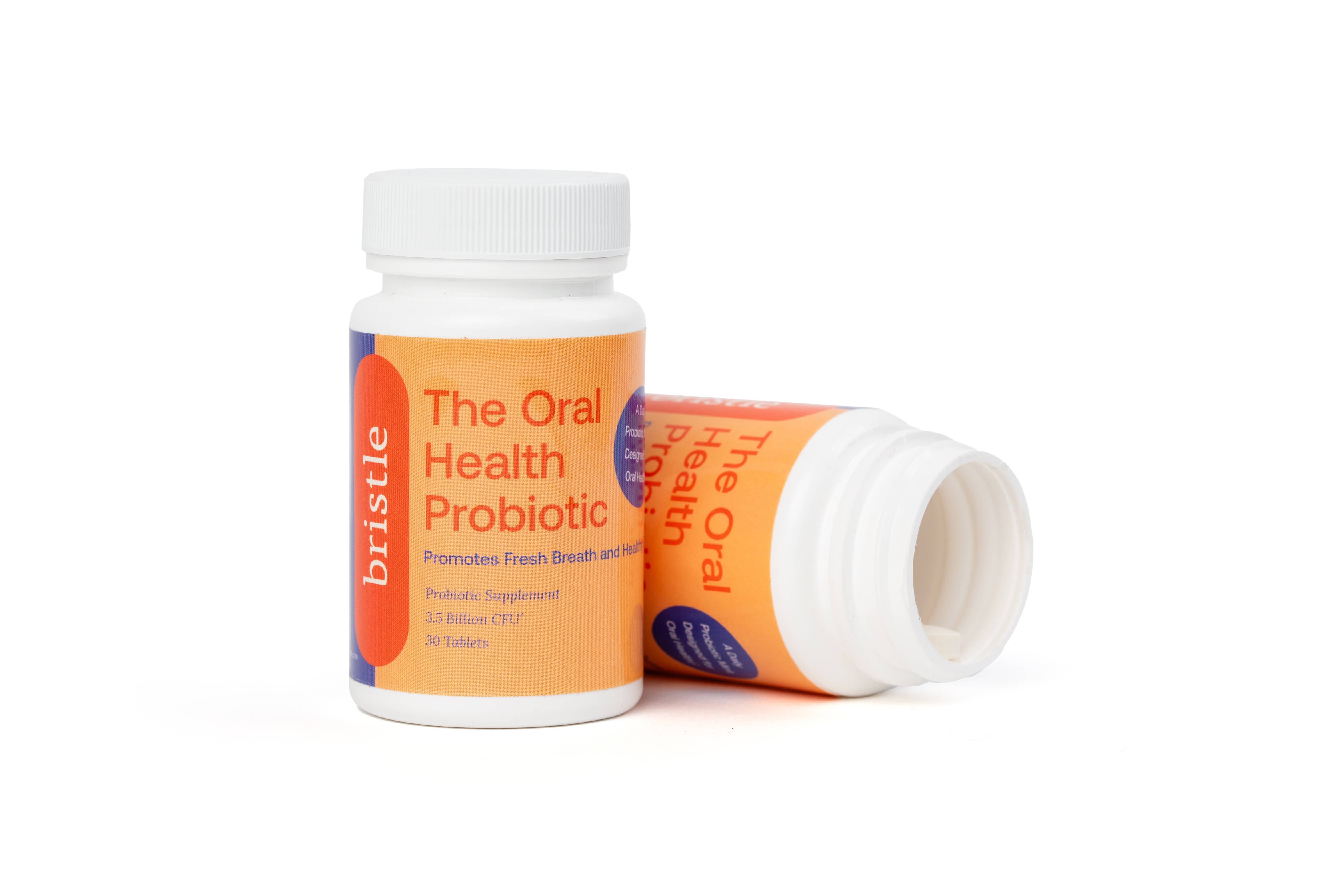
Probiotics
Some probiotics have been extensively researched, especially those containing Streptococcus salivarius, Lactobacillus reuteri, and Lactobacillus paracasei. These species have demonstrated an ability to boost commensal species, reduce harmful pathogens, and fix oral microbiome dysbiosis. You can read more about our research into dental probiotics here.
Oral hygiene
Maintaining good oral hygiene, such as routine brushing and flossing, is critical to preventing dysbiosis. Returning to the garden analogy, the oral microbiome requires constant maintenance, as weeds come in and try to invade all the time. However, pulling weeds and mulching the surface to prevent these invaders from causing damage is extremely effective. Additionally, keeping the other plants in your garden healthy can prevent diseased plants from dying, and allowing invasive plants from causing imbalance in the garden.
Want to learn more about your oral bacteria and oral health? Test your oral microbiome and receive a personalized action plan to improve your oral microbiome health with the Bristle Oral Health test.