Everyone’s mouth, including your child’s, contains a collection of microbes known as the oral microbiome. This includes both the good and bad bacteria and other microorganisms that live in the mouth. The oral microbiome in kids, like in adults, can become imbalanced. Scientists call this imbalance “dysbiosis.”
If you’ve ever wondered what causes cavities in children’s teeth, the answer is most commonly dysbiosis of the oral microbiome.
Cavities occur when certain unhealthy bacteria overgrow in the mouth. These bacteria feed on carbohydrates and sugars in our diet and release acidic byproducts as waste. As they grow, they produce more and more acid, especially when a child eats sweets and refined carbohydrates. The acid damages the enamel on a child’s teeth, leaving it wide open to cavities and even more unfriendly bacteria. This doesn’t just apply to kids. In adults, an imbalanced oral microbiome can cause cavities, as well as root canal infections, gingivitis, and is even associated with systemic illnesses such as heart disease or Alzheimer’s disease.
A number of different factors can influence whether a child’s oral microbiome is in a state of dysbiosis or whether it’s balanced and healthy. An imbalanced oral microbiome in kids is linked to a number of problems, some of them directly related to the mouth and others affecting the whole body.
Dysbiosis of the oral microbiome in kids may be linked to conditions such as:
• Cavities on children’s teeth
• Celiac disease
• Gum disease
• Pediatric appendicitis
• Pediatric inflammatory bowel disease (IBD)
• Pediatric obstructive sleep apnea
• Weight gain
What Shapes a Child’s Oral Microbiome?
A number of factors can influence whether a child’s oral microbiome is healthy or whether it’s prone to a state of dysbiosis. Some dysbiosis-related factors like genetics are out of our control, but other factors like diet can be changed to promote a healthier mouth and body.
Here are some factors that influence the oral microbiome in kids, both before and after birth.
Genetics
A child’s genetics can partially dictate the constituents of theirhis or her oral microbiome. For example, the abundance of the cavity-promoting Streptococcus mutans (S. mutans) bacteria may be driven by genetics. One study of the oral plaque microbiome in 485 twins ages 5-11 years old found that the oral microbiota was similar in twins with a similar genotype (genetic code).
Mother’s Microbiome
A mother can transfer her oral microbiome to her unborn child. The best evidence for this comes from research that shows several microorganisms found in the oral microbiome such as Streptococcus, Fusobacterium, Neisseria, Prevotella, and Porphyromonas are also found in the placentas of pregnant mothers.
This means that a mother’s dental health can make a huge difference for the dental health of her children. A mother’s diet and oral hygiene before and during pregnancy could affect her child. Dysbiosis in the mother’s mouth could lead to an imbalance in her child’s oral microbiota.
Pre-Term vs. Full-Term Birth
Whether an infant is born pre-term (before 37 weeks of pregnancy) or full-term can impact the child’s oral microbiome when the pre-term infant is low-birth weight. Pre-term infants of extremely low-birth weight were more likely to be colonized with pathogenic (harmful) microorganisms in their mouths. By week one after birth, approximately 20% of preterm and extremely low-birth weight infants were colonized with pathogens such as methicillin-resistant Staphylococcus aureus (MRSA). By week six, more than half of the preterm and extremely low-birth weight infants had mouths colonized by pathogens. This may be due to increased exposure to pathogens in the hospital’s neonatal intensive care unit.
Unlike infants born full-term, which interact with the mother, family, and home environment, pre-term and low-birth weight infants are separated from their mothers for days to months, which impacts the development of the oral microbiome.
It becomes somewhat of a vicious circle, since a mother’s poor dental health can actually lead to pre-term delivery. Mothers with periodontal (gum) disease are more likely to give birth to pre-term infants while treating periodontal disease during pregnancy reduces the risk of pre-term labor.
Delivery Method and the Oral Microbiome
A vaginal versus a C-section birth can lead to different oral microbiomes. In infants born through vaginal delivery, bacterial populations are similar to the bacterial communities found in the mothers’ vagina, with bacteria such as Lactobacillus, Prevotella, and Sneathia. On the other hand, infants born through C-section have bacterial populations that are similar to those found on the mother’s skin such as Staphylococcus, Corynebacterium, Slackia, Veillonella, and Propionibacterium.
One study showed that the differences in oral microbiota between babies born vaginally and those born through C-section went away by one week after birth.
Not all study findings agree, so more research is needed in this area.
Teething
Everything begins to change once a child starts growing primary teeth. Oral bacteria now have something more to adhere to. A greater number of species (alpha diversity) starts to develop with different types of bacteria predominating compared to a toothless mouth. S. mutans becomes highly prevalent as it prefers to stick to teeth rather than gum surfaces.
Other Family Members and Friends
Family members that have direct contact with a child contribute to their oral microbiome. They will acquire similar microbes to others in their household or environment. When children kiss their parents on the mouth, they can share oral bacterial communities. When family members have healthy microbiomes containing Streptococcus gorgonii and Streptococcus sanguinis, it can promote dental health and decrease risk of cavities in children.
This also goes for undesirable bacteria. People in close contact with children can transmit the cavity-promoting bacteria S. mutans. Fathers can also transmit this type of bacteria to their children. Furthermore, one analysis found that 55% of grandmothers included in the study transmitted S. mutans to their grandchildren. Other studies have found that kids can acquire cavity-promoting bacteria from playmates in nursery and elementary schools.
Formula vs. Breastfeeding
The characteristics of the oral microbiota in formula-fed and breastfed infants are different. S. mutans is more common in formula-fed infants compared to those who were breastfed and bottle-fed infants have more cavities than those who were breastfed.
There are several explanations for the difference between formula feeding and breastfeeding:
• Oral bacteria could be transmitted differently depending on whether formula or breastmilk is used.
• Bacteria may adhere differently to the oral cavity depending on whether formula or breastmilk is used.
• Oral bacteria use the prebiotic carbohydrates in breastmilk and formula differently.
• Breastfeeding boosts the infant’s innate immunity, which reduces the ability of pathogenic bacteria to colonize the mouth.
However, some studies show that the duration of breastfeeding matters. Infants who are breastfed for more than 12 months might actually have an increased risk of cavities.
The Mother’s Diet
During pregnancy and breastfeeding, the type of diet a mother eats can affect her own and her baby’s oral microbiome. For example, drinking low-calorie diet drinks with artificial sweeteners or sucralose while breastfeeding may lead to vomiting in the infant and an altered gut microbiome, which is often connected to the oral microbiome. Breastfed infants of mothers who eat a higher amount of fat and saturated fat and a lower intake of healthy carbohydrates are more likely to develop allergies.
While breastfeeding, it’s best to avoid sodas, sweets, and processed carbohydrates like pasta and bread and opt for lean meats, vegetables, and fruits. Mothers who eat healthy while breastfeeding influence their child’s food choices down the road. Breastfed infants of mothers who eat lots of vegetables eat more vegetables later in life, possibly due to exposure to vegetable flavors early in life.
Your Child’s Diet
When children stop breastfeeding and move on to solid foods, what they eat and drink influences their microbiomes. Avoiding sweets, sodas, and processed food leads to a healthy oral microbiome. Choose whole foods, fiber, lean meats, nuts, vegetables, and fruits.
“Baby bottle tooth decay” is a term that describes early childhood cavities caused by prolonged exposure to sweetened fluids like milk, formula, or fruit juice. Research has found that kids who drink a lot of sugar-sweetened beverages have an altered oral microbiota that contains more cavity-causing bacteria. Children who develop cavities also have a higher abundance of two types of bacteria (Paludibacter and Labrenzia) that metabolize sugar and make the saliva more acidic, leading to cavities in kids.
Nutrition
Ensuring your child’s diet contains critical nutrients is another important way to keep the oral microbiome healthy. Vitamin D is important for dental health in children and adults. It helps the body absorb calcium, a mineral that comprises tooth enamel. Vitamin D also repairs damaged dentin, which is located under the tooth enamel and protects the blood supply and nerves inside the teeth. Your child can get enough vitamin D by spending time out in the sun and by supplementing with this nutrient.
Vitamin E maintains the immune system in your children’s mouth to protect against cavities and gum disease. Vitamin E acts as an antioxidant and when given to animals together with zinc, it reduced cavities, likely due to reducing lactic acid buildup in dental plaque.
Vitamin K2 is another nutrient important in calcium metabolism and may protect against tooth decay.
Oral Hygiene
Teeth brushing, flossing daily, and visiting the dentist for regular cleanings are important ways to make sure the oral microbiota in kids stays healthy and balanced. Choose toothbrushes with rounded bristle tips that have a smooth surface to avoid injuring the gums.
Nasal Breathing
When children breathe through the mouth instead of the nose, it can alter the oral and nasal microbiota and cause certain pathogens to flourish. Mouth breathing also changes the saliva in a way that’s not conducive to a healthy mouth.
Antibiotics
Antibiotics, whether prescribed to the mother during pregnancy or breastfeeding or to infants or children, can alter the oral microbiota. Research shows that when mothers are given antibiotics during pregnancy it changes their child’s oral microbiome. Taking probiotics at the same time as antibiotics may reduce some of the adverse effects of the antibiotics and reduce the risk of oral dysbiosis.
Other Strategies to Maintain Children’s Oral Health
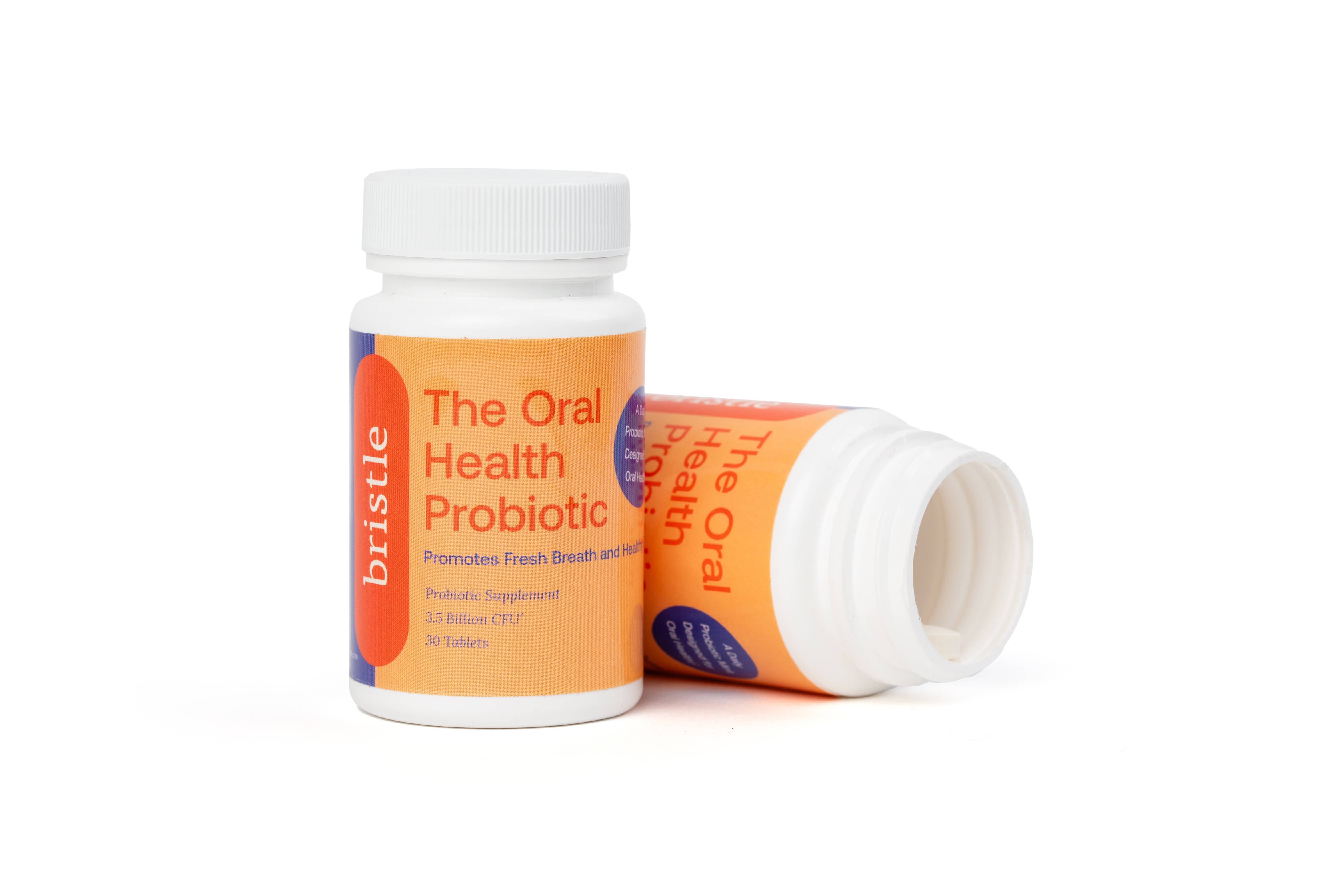
Probiotics
Probiotic supplements contain beneficial bacteria that balance the oral microbiome and keep harmful bacteria at bay. Chewable probiotics are ideal options for younger children who have problems swallowing pills.
Xylitol Gum
This type of gum contains a healthy sugar substitute called xylitol found in many fruits and vegetables. Some studies have found xylitol may reduce the numbers of cavity-causing bacteria in dental plaque and saliva. In one study, children of mothers who chewed xylitol gum in the later stages of pregnancy were less likely to develop cavities.
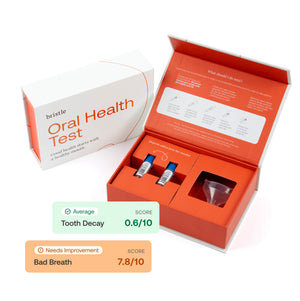
Salivary Oral Microbiome Testing
Testing the oral microbiome in both you and your children is an effective way to measure 100-plus bacteria that contribute to cavities, bad breath, and gum inflammation. Personalized strategies to improve you and your child’s oral microbiome accompany the oral microbiome testing.
Prevent Cavities in Children
The oral microbiome is a major player in children’s oral health and whole-body health. Even if you have problems with oral health, your child doesn’t have to inherit them! Children begin developing their oral microbiomes before birth. Mothers, fathers, and caregivers can make choices to promote a healthy oral microbiome that prevents cavities in children. With plentiful amounts of beneficial or harmless microbes in the mouth, infections are less likely to take hold. A healthy and balanced oral microbiome will set the stage for a healthy child who grows into a healthy adult.
About the author
Cass Nelson-Dooley, MS, has over a decade of experience teaching doctors about integrative and functional laboratory results. In 2013, she started Health First Consulting, LLC, a medical communications company with the mission to improve human health using the written word. She created innovative videos and patient education handouts to improve practice efficiency and motivate patients. Ms. Nelson-Dooley is the author of Heal Your Oral Microbiome and has published case studies, book chapters, and journal articles about natural medicine, nutrition, and laboratory testing. Learn more at www.healthfirstconsulting.com.