Research now shows that bacteria in the mouth can actually travel to the gut and cause gut inflammation. The mouth and gut interact via a pathway called the oral-gut axis, where the oral microbiome and gut microbiome are connected in an intertwined network that also involves the immune system. Scientists are now uncovering the ways that the microbes in the mouth and gut interact to promote health or disease. In this article we summarize current research on how the oral microbiome can cause Inflammatory Bowel Disease.
What causes IBD?
The exact cause of IBD is still not entirely clear, but research has shown that gut microbiome dysbiosis is a primary feature in people with IBD. People with IBD are in a constant state of inflammation, where the immune system is triggered by antigens in the gut, causing symptoms such as diarrhea, bloating, abdominal pain, and fatigue.
Scientists have found that this persistent inflammation is correlated with changes in both the oral microbiome and gut microbiome. Normally, these microbiomes are stable, and in homeostasis. However, for people with disease, the microbiomes are imbalanced, also known as dysbiosis. Additionally, research has shown that oral dysbiosis and gut dysbiosis may preempt disease, and specific bacteria in the mouth and gut can cause inflammation.
Oral microbiome dysbiosis and IBD
Research has shown that people with IBD have specific changes to their oral microbiome. People with IBD exhibit increased oral microbiome dysbiosis compared to healthy people. Additionally, people with gum disease are 50% more likely to have IBD.
New research now shows that specific bacteria in the mouth can actually migrate to the gut either via the gastrointestinal tract through the stomach, or through the circulatory system.
How oral bacteria can travel to the gut
Normally, your gums act as a first line of defense in keeping bacteria out of your body. However, oral microbiome dysbiosis causes gum inflammation, breaking that barrier and allowing bacteria into your body. These bacteria are more likely to translocate to the intestine in people with gum inflammation, and people with oral microbiome dysbiosis.
In the past decade, several studies have shown that gum disease pathogens, such as, Porphyromonas gingivalis, dramatically worsen IBD symptoms (1, 2, 3, 4, 5, 6, 7). Scientists proposed that P. gingivalis and other pathogens trigger gum inflammation in the mouth, which allows other bacteria, such as Fusobacterium nucleatum, to migrate through the circulatory system and cause disease elsewhere in the body. High abundance of P. gingivalis is a signature of oral microbiome dysbiosis, and causes gum disease.
Oral bacteria can also move from the mouth to the gut via the gastrointestinal tract. Some of these bacteria are acid-tolerant, and able to survive the low pH of the stomach to reach the intestine. Most of the time these bacteria are unable to colonize the gut, however in some cases, the introduction of these bacteria disturbs the existing gut microbiome, and causes gut dysbiosis. The determinants for who are able to be colonized by bacteria from the mouth is still unclear.

How oral bacteria cause gut inflammation
After bacteria in the mouth migrate to the gut, they can colonize where they normally wouldn’t, called ectopic colonization. In recent years, multiple studies have demonstrated how oral microbiome dysbiosis can cause gut disease.
A study in 2011 found that Fusobacterium nucleatum, a bacteria normally in the mouth, correlated with IBD status, and people with high abundance of F. nucleatum are at higher risk of IBD. Later, a study in 2019 found that F. nucleatum accumulated to specific regions in the gut, and those regions had extremely high levels of inflammation. Later, a study showed that F. nucleatum was an early marker of gut dysbiosis. F. nucleatum was also found to lead to an increased risk of colorectal cancer.
A study in 2017 found that Klebsiella species, specific bacteria that are normally found in the mouth, can end up in the gut, colonize, and cause inflammation. They found that Klebsiella pneumoniae, and other Klebsiella species were involved in IBD progression, and disease. These bacteria in the mouth acted as a reservoir that caused persistent inflammation.
In 2020, scientists found that Klebsiella and Enterobacter species not only migrate from the mouth to the gut to cause inflammation, but they also caused immune cells in the mouth to become pro-inflammatory. These immune cells were then found to also migrate to the gut where they exacerbated gut inflammation.
More research is underway to determine the mechanisms of this cross-colonization from the mouth to the gut. It remains to be seen which types of gut microbiomes are more resistant to colonization by bacteria in the oral microbiome. Additionally, more research has to be done to determine whether removing these species from the oral microbiome can reduce risk of IBD.
Summary: bacteria in the oral microbiome can cause gut inflammation
Together, this recent data shows that oral microbiome dysbiosis can lead to gut diseases like IBD and Crohn's. The presence of gum disease-causing pathogens allows for pro-inflammatory bacteria in the oral microbiome to penetrate into the body, down to the gut, and cause severe gut inflammation.
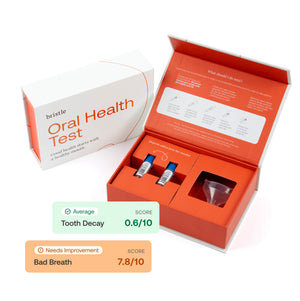
Want to learn more about your oral bacteria how they may be impacting your gut health? Test your oral microbiome with the Bristle Oral Health test.