Key points
Cancer is a leading global killer, taking an estimated 10 million lives worldwide in 2020 and diagnosed in over 19 million new cases. In the US, 1 in 3 people will be diagnosed with cancer and about half of those people will die from it. Very likely you or someone you know has been affected by cancer.
You already know certain risk factors, like smoking, lead to cancer. But did you know that a large, growing body of research is connecting poor oral health and a dysbiotic oral microbiome to cancers throughout the body?
Here we’ll take a close look at how gum disease may influence cancer and what members of the oral microbiome play a role in tumor development.
Gum disease and cancer
Many epidemiological studies over the years have reported associations between periodontal (gum) disease and cancer. Since half of adults in the US have periodontal disease, the public health impact could be huge if that relationship is causal. If so, you could potentially reduce the risk of developing cancer or slow it down by preventing or treating gum disease.
Overall cancer risk
A meta-analysis of multiple studies reported a 14 - 20% increase in total cancer risk associated with gum disease, adjusting for smoking status — a major risk factor for both diseases.
Another large prospective cohort study followed 7466 people, who underwent dental examinations and had no prior cancer history. Measuring probing depth and gingival recession — the same measures your dentist takes at your checkup — and tracking whether or not the participants developed cancer, researchers found that severe periodontal disease elevated overall cancer risk.
What is gum disease?
Periodontal (gum) disease is largely a chronic inflammatory disease driven by a pathogenic oral microbial community growing below the gum line. When we’re healthy, our immune systems can clear this microbial infection. Careful dental hygiene (flossing, water flossing, etc.) disrupts the surface biofilms that protect these bacteria, making it easier for your immune system to clear the rest.
During severe periodontal disease, the immune system responds erratically to the dysbiotic oral microbiome, producing chronic inflammation that can destroy bone and gum tissue, leading to bleeding and tooth loss. The oral pathogens persist, triggering a vicious cycle of chronic inflammation.
What causes cancer?
Driven by changes to genes (mutations or variants) that control the way our cells normally reproduce, cancer develops when some of our cells grow unchecked and then spread into surrounding tissues. Certain genetic variants enable these rogue cells’ aggressive growth and ability to escape our immune system checks on them.
Cancer can arise from:
Since chronic inflammation and microbial infection are both hallmarks of periodontal disease, it isn’t surprising scientists and dentists are now paying closer attention to this possible connection.

Cancers in and around the mouth
Oral and oropharyngeal cancers most often occur on the tongue, tonsils, oropharynx, gums, roof and floor of the mouth, and the lips. The vast majority of oral and oropharyngeal cancers are squamous cell carcinomas. Squamous cells are thin, flat cells that line the inside of our lips and oral cavity. Non-squamous cell types can also develop into cancer, but these are a mixed group of much rarer cancers.
Major risk factors include tobacco use, alcohol consumption, and advanced age. Ethanol and nicotine seem to be direct carcinogens. Age, of course, is associated with many risk factors: weaker immune response, accumulated mutations, long-term exposure to carcinogens, etc.
However, some people without these risk factors still develop oral and oropharyngeal cancers. What other factors might influence these cancers? Infectious microbes are other possible triggers.
For example, infection by human papillomavirus (HPV) — especially HPV subtype 16 — is strongly associated with oropharyngeal cancers. HPV infection also increases your risk of oral squamous cell carcinoma by up to threefold. However, some people infected with HPV will never develop cancers, while others may develop them only much later after infection. Other viruses have also been associated with oral cancers, specifically herpes simplex (HSV), Epstein-Barr (EBV), and Hepatitis C (HCV).
It’s not just viruses; several studies of oral cancer samples summarized here have observed increases in certain species of oral bacteria, including Capnocytophaga gingivalis, Prevotella spp., Filofactor alocis, and Fusobacterium spp. (which we'll discuss more later). However, it is still unclear if oral cancer itself shapes these microbiome changes or the other way around.
Periodontal disease also has a small but significant association to oral cancer, further signaling the need to prevent oral dysbiosis.
Cancers beyond the mouth
Periodontal disease itself or related dysbiotic oral microbiome shifts have been associated with other cancers, including:

It is important to note that although these studies suggest an association between periodontal disease or oral microbiome changes and cancer, they do not clearly indicate a causal relationship and all the mechanisms driving cancer development are likely multifaceted and complex. Also, studies range widely in how they measure periodontal disease, and results can vary between different populations and places. Breast cancer, for example, shows only a low or moderate association with periodontal disease.
Despite the challenges and variation in these studies, gum disease consistently demonstrates association with a few cancers — one being colorectal cancer (CRC).
Since the mouth is the gateway to the rest of the body, especially the gastrointestinal system, it isn’t surprising to see associations between periodontal disease and cancers originating in the gut. Moreover, one oral bacterium, Fusobacterium nucleatum, is increasingly being implicated in colorectal cancer.
A strong connection between a common oral microbe and colorectal cancer
In a healthy mouth, F. nucleatum is a peaceful, common member of the oral microbiome – its numbers and potential to activate a strong inflammatory response kept in check.
However, F. nucleatum increases rapidly in numbers during the early stages of periodontal disease, helping dental plaque grow and organize by connecting early colonizers of the biofilm, like Streptococcus spp., to anaerobic species associated with a dysbiotic microbial community, like Porphyromonas gingivalis. This ability, which allows F. nucleatum to efficiently stick to other bacterial species in the dental plaque, also enables it to attach to and invade human host cells.
Now researchers understand more about how this bacterium, adapted for life in the oral cavity, influences disease in other body sites. More than just a passive microbial “passenger” along for the ride beyond the oral environment, F. nucleatum likely drives tumor development in CRC.
Although a common oral species, F. nucleatum is found in only very low levels in a healthy gut. Many studies have observed F. nucleatum enriched in CRC tumors. From CRC tumor biopsies, researchers have identified oral F. nucleatum strains while other researchers have even cultured live F. nucleatum. Moreover, patients with high numbers of F. nucleatum in CRC tissue face worse prognosis.
Once near intestinal tissue, F. nucleatum can influence CRC growth in many ways. It can trigger intestinal epithelial cells to grow out of control by overactivating multiple cell signaling pathways. It can also block tumor-killing abilities of our immune systems’ natural killer cells and T-cells and even induce resistance to life-saving chemotherapy.
Understanding how the oral microbiome changes during cancer and identifying cancer and patient-specific biomarkers may help scientists one day develop better predictive screening tests for colorectal cancer.
How does F. nucleatum find its way out of the mouth and into places it doesn’t belong?
F. nucleatum likely travels to other body sites by moving:
F. nucleatum has even greater access to the bloodstream during periodontal disease, where gum tissue and bone are destroyed by inflammation and new paths to the circulatory system are created. Therefore, promoting a healthy, balanced oral microbiome may limit the ability of any oral bacteria to reach other body sites that may cause disease.
How you can lower your cancer risk
Although we cannot change our genetics, family history or aging, we can control behaviors and exposures which may affect our risk for cancers associated with the oral microbiome.
Early detection
Oral and oropharyngeal cancers are difficult to detect in early stages and there are currently no routine screening tests. However, dentists and dental hygienists are on the front lines looking for early signs of oral cancer, like leukoplakia, lichen planus, or unhealing sores. Getting regular checkups by dentists and dental hygienists who are trained to look for these signs may help identify oral and oropharyngeal cancers in early stages – when treatment is most effective.
In 2021, gut microbiome company Viome developed a saliva test to screen for oral and oropharyngeal cancers using a metatranscriptomic sequencing approach. This screening test is one example of how microbiome testing methods can be used to improve human health.
Since all colorectal cancers start as abnormal growths, or polyps, in the colon or rectum, routine screening tests starting at age 45 can find these polyps, allowing doctors to remove them before they become cancerous or prescribe treatment at an early stage of colorectal cancer. Such tests include colonoscopy and more recently, fecal immunochemical tests (FITs).
Consider vaccination
Although the HPV vaccine was originally developed to prevent cervical and other cancers related to the reproductive system, it also protects against oral infection by HPV types, especially HPV subtype 16, that cause oropharyngeal cancer. The CDC recommends routine vaccination at 11 to 12 years old and for everyone up to age 26.
Make healthy choices
Periodontal disease, inflammation, and cancer share similar environmental risk factors. Reduce your risk by:
Maintaining or improving your oral health
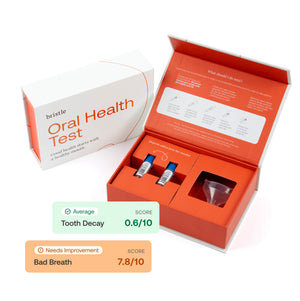
In addition to routine dental checkups and cleanings, maintaining a healthy oral microbiome is vital to reducing your chances of developing oral diseases. You can learn a lot by understanding the ecosystem of bacteria that are living in your mouth. Send us a sample, and we'll analyze it for you. You'll get a complete report about your oral microbiome and what it means for the balance of your bacterial companions, what it means for your health, as well as personalized recommendations on how to use that knowledge to maximize your oral health!